
The Ohio Department of Medicaid (ODM) is launching the Next Generation MyCare Program in January 2026. If you or your loved one currently receive services through MyCare Ohio—or are eligible for both Medicare and Medicaid—this update is designed to make managing benefits easier, give you more personalized care, and expand services statewide.
This post will explain the key changes, how they impact members and caregivers, and how to prepare for the transition.
What is MyCare Ohio?
MyCare Ohio is a managed care program for Ohioans who qualify for both Medicare (the federal health insurance program for seniors and individuals with disabilities) and Medicaid (Ohio’s state-run medical program for people with low income or disabilities).
At its core, MyCare Ohio combines benefits from both Medicaid and Medicare into one streamlined program, eliminating the need for members to manage two separate systems.
Here’s how it works:
- You pick a managed care plan: Options are available based on your location and include both Medicaid and Medicare services.
- Integrated services: These plans provide coverage for everything, including medical care, behavioral health services, and long-term care supports like in-home personal care assistance.
- Dedicated care coordinators: Members are assigned a care manager who helps schedule appointments, handle medication and prescriptions, navigate covered services, and ensure you get the support you need.
NextGen MyCare - What you need to know for 2026
Why Is the Program Changing?
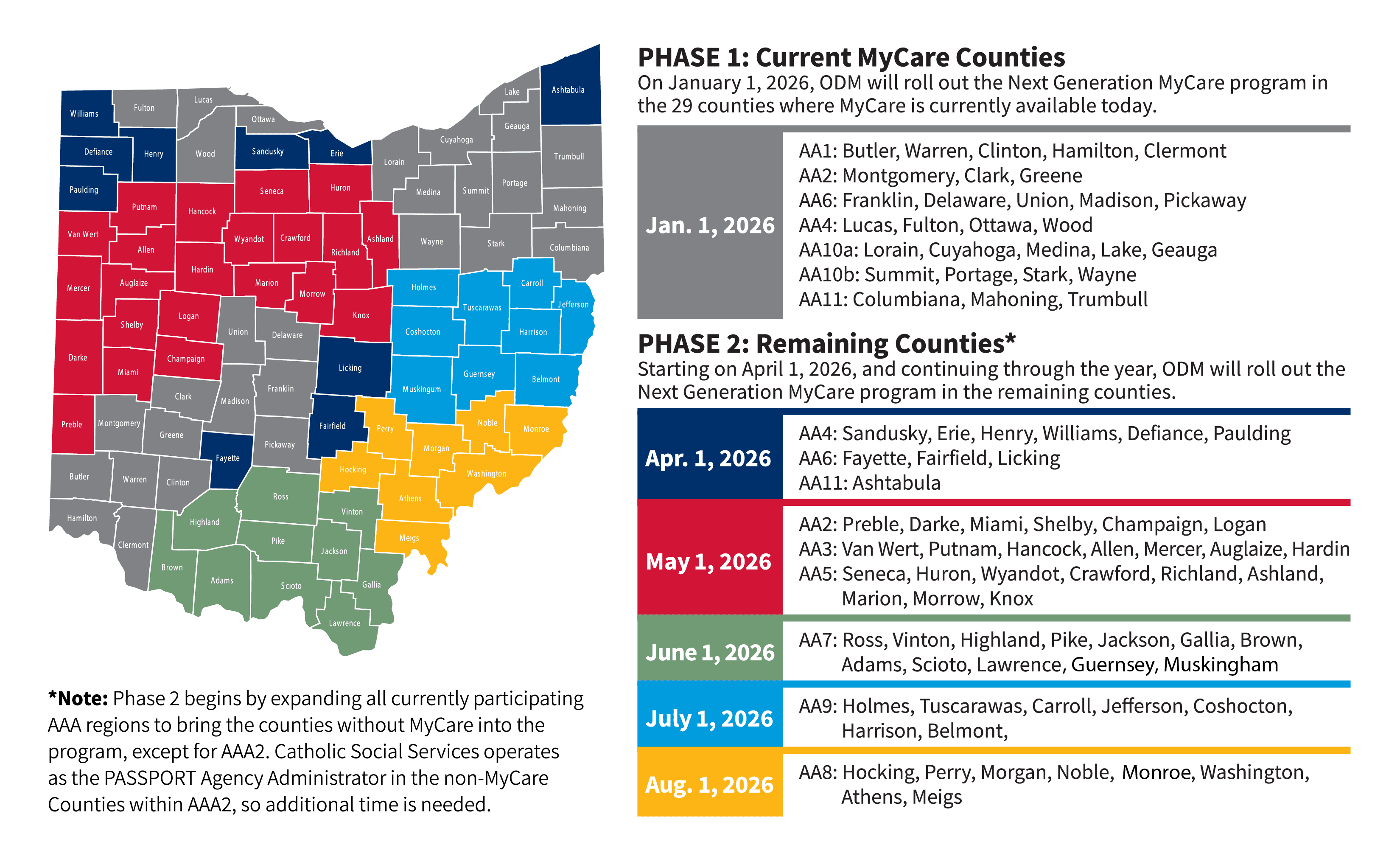
Starting January 1, 2026, Ohio Medicaid is transitioning to the Next Generation MyCare Program to improve access, personalize services, and make navigating Medicaid and Medicare easier than ever. This update will start in 29 counties already using MyCare before expanding statewide later in 2026.
What Are the Changes and How Do They Affect Members?
The Next Generation MyCare Program introduces important changes to eligibility, provider selection, and plan management. Here are the highlights:
- Age Requirement Change
The minimum age for eligibility will increase from 18+ to 21+ starting in January 2026. Members under 21 will need to explore alternate Medicaid options. - Simplified Care Coordination
Every member will have one care coordinator dedicated to:- Scheduling appointments.
- Managing medications and prescriptions.
- Connecting members to additional resources like home-delivered meals or personal care aides.
If a member qualifies for MyCare waiver services, they’ll have access to a waiver service coordinator who specializes in long-term care programs like home modifications and in-home caregiving.
- Updated Managed Care Providers
The NextGen program selects new managed care organizations (MCOs) to oversee services. The four providers chosen include:- Anthem Blue Cross and Blue Shield
- Buckeye Health Plan
- CareSource
- Molina Healthcare of Ohio
- Plan Selection and Transition
- Aetna and UnitedHealthcare members: You will need to select a new provider from the four chosen MCOs before January 2026. You will receive enrollment details in the mail before the NextGen Program starts.
- Buckeye, CareSource, or Molina members: You will renew automatically unless you actively choose a different provider.
- Waiver Service Continuity
Waiver services (e.g., personal care aides, durable medical equipment, and home modifications) will not be interrupted during the transition. Current eligibility requirements for waivers remain the same. - Enrollment Information
Members will receive plan enrollment details in the mail before the NextGen program year starts. It’s important to review this information carefully and take appropriate action (if needed) before January 2026.
Key Takeaway: Members currently enrolled in MyCare Ohio will not lose benefits during the transition. The goal is a seamless shift to NextGen plans without any disruption in coverage.
Rollout Plan
Below is the expected rollout plan coming from medicaid.ohio.gov.
FAQs for Family Caregivers
- Will family caregivers be paid under NextGen MyCare?
Yes! Family caregivers may qualify for compensation if they provide services like personal care under MyCare waiver programs. Contact your waiver service coordinator for additional support. - Do I need to select a new plan?
You must choose a new plan if you’re currently with Aetna or UnitedHealthcare. Members with Buckeye, CareSource, or Molina will transition automatically unless a new plan is selected. - Will waiver services change under NextGen?
No. Waiver services, eligibility criteria, and access will continue as before under the updated program.
Where to get more information
- MyCare Additional Information from ODM
- Best resource for all things MyCare and specific details on each of the changes.
- Questions about eligibility or switching plans?
- Call the Ohio Medicaid Consumer Hotline (800-324-8680).
- Using Medicaid waiver services like PASSPORT?
- Call the Area Agency on Aging (866-243-5678).
- Want general NextGen program info?
- Email: MyCareConversionQuestions@medicaid.ohio.gov.
- Exploring self-direction services?
- Email: self-direction@medicaid.ohio.gov.
- Need plan-specific help?
- Call your managed care plan’s hotline: Anthem, Buckeye, CareSource, or Molina.
- Hotlines here:
- Anthem Blue Cross and Blue Shield: 833-727-2169
- Buckeye Health Plan: 855-445-3562
- CareSource: 855-475-3163
- Molina Healthcare of Ohio: 866-856-8295
Get support for your caregiving journey today
We help you get certified as a caregiver and enroll in federal programs to receive compensation for family caregiving. Start your CareOasis journey now.